Understanding Quantitative LH Monitoring — and Why It Matters
If you’ve ever used an ovulation test, you’ve probably seen a simple “yes” or “no” result telling you whether you’re “surging.” But your hormones aren’t that simple.
Luteinizing hormone, or LH, is one of the main messengers that controls your cycle. It works with other hormones like FSH, estrogen, and progesterone to mature an egg and trigger ovulation. When LH rises sharply—usually about 24–36 hours before ovulation—it signals your body that it’s time to release an egg.
Most at-home ovulation kits only tell you when your LH passes a certain threshold. The problem? Not everyone’s “normal” is the same. Hormones rise and fall differently for each person and from one cycle to the next.
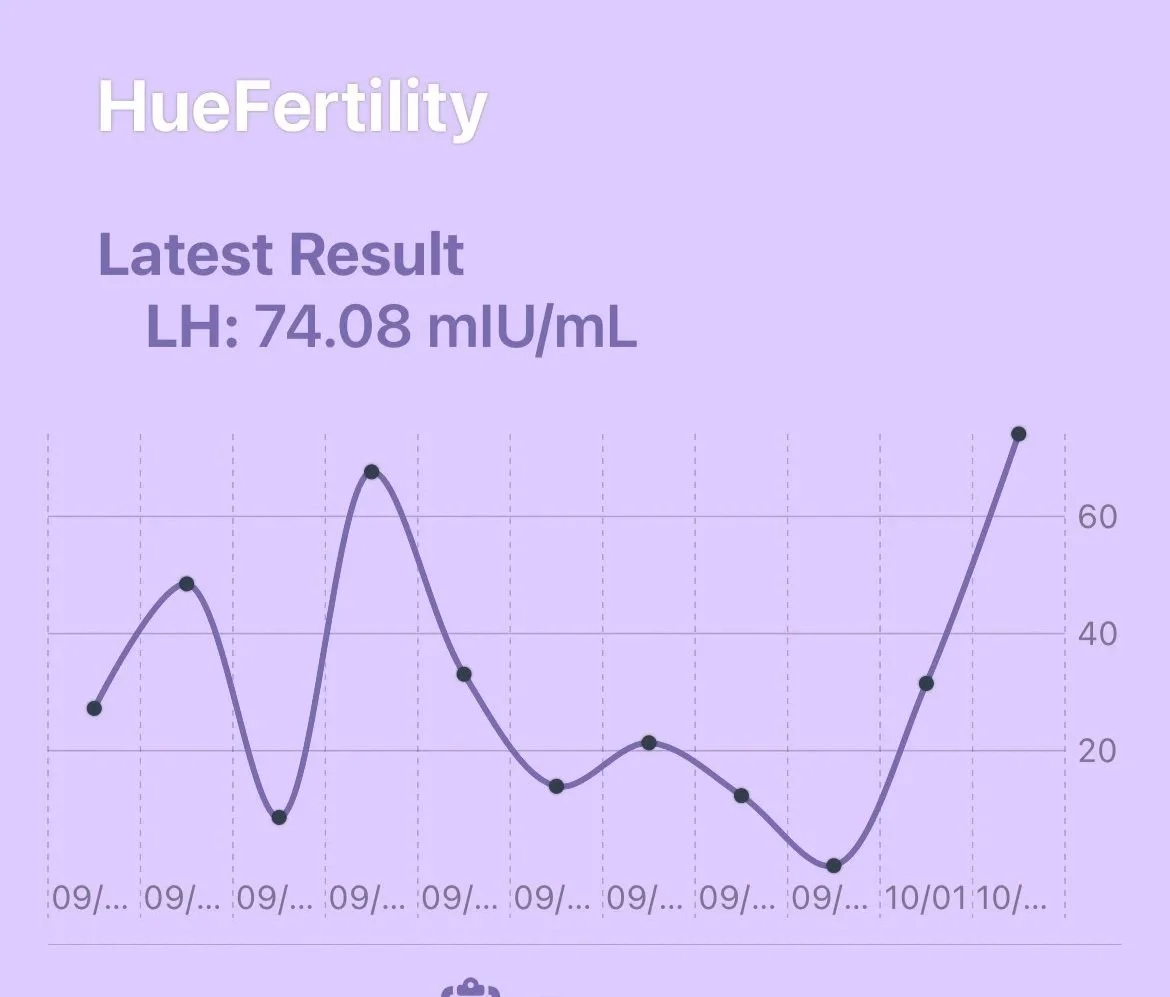
That’s where quantitative LH monitoring comes in. Instead of a basic yes/no result, it measures your actual LH levels, showing how they change day to day. That extra detail helps you truly understand what’s happening in your body.
Why More Detailed LH Data Helps
Here’s what you gain when you track LH quantitatively:
1. You can spot a trend, not just a spike.
Instead of waiting for a single “positive” test, you can watch your LH slowly rise, peak, and fall—seeing the full story of your cycle.
2. You learn your personal baseline.
Some people naturally have higher or lower LH levels. Quantitative tracking helps you see what’s normal for you.
3. You can confirm ovulation more confidently.
Seeing the rise and fall in LH helps you know when ovulation likely happened, not just when it might be about to.
4. You notice when something seems off.
If LH stays high for too long, rises in small waves, or doesn’t peak clearly, it might signal a hormonal imbalance that’s worth understanding with your provider.
5. You can look at long-term patterns.
Tracking over several months can reveal how stress, lifestyle, or treatments affect your cycle over time.
Simply put: the more data you have, the better you can understand your body—and the less you have to guess.
How It Helps in PCOS and Postpartum
PCOS (Polycystic Ovary Syndrome)
If you have PCOS, your hormone levels often don’t follow the “standard” pattern. LH may stay higher than average or rise multiple times in one cycle, which can confuse regular ovulation kits.
A quantitative approach helps you:
See smaller, meaningful increases in LH that might not trigger a traditional test.
Identify when multiple LH peaks happen—and which one is most likely linked to real ovulation.
Track how lifestyle changes or treatments affect your hormones across cycles.
According to the American Society for Reproductive Medicine, individualized hormone tracking is especially valuable for people with PCOS because it gives a clearer picture of what your body is actually doing, rather than relying on one-size-fits-all thresholds.
Postpartum (After Having a Baby)
The months after giving birth can bring unpredictable hormone patterns. Prolactin (especially while breastfeeding), sleep changes, and stress can all delay or suppress ovulation.
In this stage, LH tracking helps you:
Notice when your hormones start “waking up” again after birth.
Spot the difference between small, early rises in LH and a true ovulatory surge.
Understand how your body is transitioning back to regular cycles.
Because postpartum cycles can be irregular or unpredictable, this kind of detailed monitoring provides a more accurate picture than traditional kits.
What “Double Peaks” Mean
Sometimes you might see two LH peaks in one cycle. It’s not as strange as it sounds! There are a few reasons this happens:
The first rise doesn’t lead to ovulation. Your body may start gearing up but doesn’t release an egg until a later LH rise.
Your hormones pulse naturally. LH is released in waves throughout the day, so you may catch smaller “mini peaks.”
You may be growing more than one follicle. Sometimes the body makes more than one attempt at ovulation.
Testing or hydration differences. Drinking a lot of water or testing at different times can cause small variations.
Seeing multiple peaks doesn’t mean anything’s “wrong,” but it does show why having more than one data point matters. Tracking continuously helps you tell which peak represents true ovulation.
Why One Test Isn’t Always Enough
Ovulation doesn’t always happen on a schedule. The LH surge can last anywhere from a few hours to a couple of days—and may happen earlier or later than expected.
If you only test once or twice, you might miss the real peak entirely. Quantitative tracking gives you the full curve, making it easier to tell whether:
You actually caught the surge
LH stayed high without falling (which might suggest a hormonal imbalance)
Your surge was weaker or shorter than usual
This kind of tracking also pairs beautifully with other clues—like temperature shifts or changes in cervical mucus—to build a complete understanding of your cycle.
Beyond Ovulation: What LH Can Tell You About Health
LH data isn’t just about fertility. Over time, your hormonal patterns can tell you a lot about your overall health.
Changes in your LH curve may point to stress, thyroid changes, or perimenopause.
Tracking over months can show how your hormones respond to new habits, supplements, or medications.
Noticing missing surges may help identify cycles where ovulation didn’t happen, even if you had bleeding.
Your hormones are like a monthly report card from your body—and LH is one of the clearest signals in that report.
The Bottom Line
Quantitative LH monitoring gives you more than a yes/no answer—it gives you insight.
It shows the whole rhythm of your hormones.
It helps confirm when ovulation really happens.
It provides valuable feedback for PCOS, postpartum, and irregular cycles.
It connects fertility tracking to overall hormonal health.
When you can see the data clearly, you can make decisions with confidence—and that’s what truly personalized fertility looks like.
References
American Society for Reproductive Medicine (ASRM). (2023). Evaluation and Treatment of Polycystic Ovary Syndrome.
Li, X., et al. (2022). Complete hormonal cycle mapping: New insights from at-home quantitative hormone testing. Reproductive Biology and Endocrinology
Gnoth, C., et al. (2003). Definition and prevalence of subfertile cycles in normally fertile women. Human Reproduction.
Su, H. W., et al. (2017). Detection of ovulation: A review of currently available methods. Bioengineering & Translational Medicine.
Rosenfield, R. L., & Ehrmann, D. A. (2016). The pathogenesis of PCOS: Functional ovarian hyperandrogenism revisited. Endocrine Reviews.